Dr Munir Somji presents a case study of a patient treated with dermal filler for a tear trough concern
The tear trough is a common ageing concern for many aesthetic patients, as it tends to be the first thing people notice when making eye contact with one another.
Infraorbital hollowing can give patients a fatigued appearance, perhaps despite them having sufficient rest. In my experience, treatment for this area has extremely high satisfaction ratings and gives an instant ‘freshness’ that many patients crave. It is, however, a difficult area to treat, as detailed knowledge of the anatomy coupled with an inherent knowledge of dermal filler rheology is required. The ‘tear trough deformity’ was first coined by Flowers in 1993. ¹ In general, it can be described as a periorbital hollow that extends obliquely from the medical canthus to the midpupillary line. Any depression lateral to this is termed the ‘palpebromalar groove’, ‘lid-cheek junction’ or ‘nasojugal groove’. For the purpose of this article, we will be discussing techniques for rejuvenation of the tear trough area.² Since 1993, there have been numerous classifications of the deformity of the tear trough area and its aetiology.³ The classification that aids my clinical practice is the Tear Trough Rating Scale (TTRS),4 which gives practitioners a way to quantitatively assign the tear trough deformity, measuring the volume of prolapsed fat, skin rhytidosis, hyperpigmentation and depth of tear trough. Explaining this scale to patients tends to give them a better understanding of the results they can expect to obtain from a tear trough augmentation treatment. I also find that it provides practitioners with the perfect tool to manage expectations. For example, if a patient has a higher degree of pigmentation than depth of tear trough, they may be better suited to different treatments to achieve maximal results. Treatments for pigmentation such as skin peels and daily application of topical tyrosinase inhibitors would be appropriate.
Case study
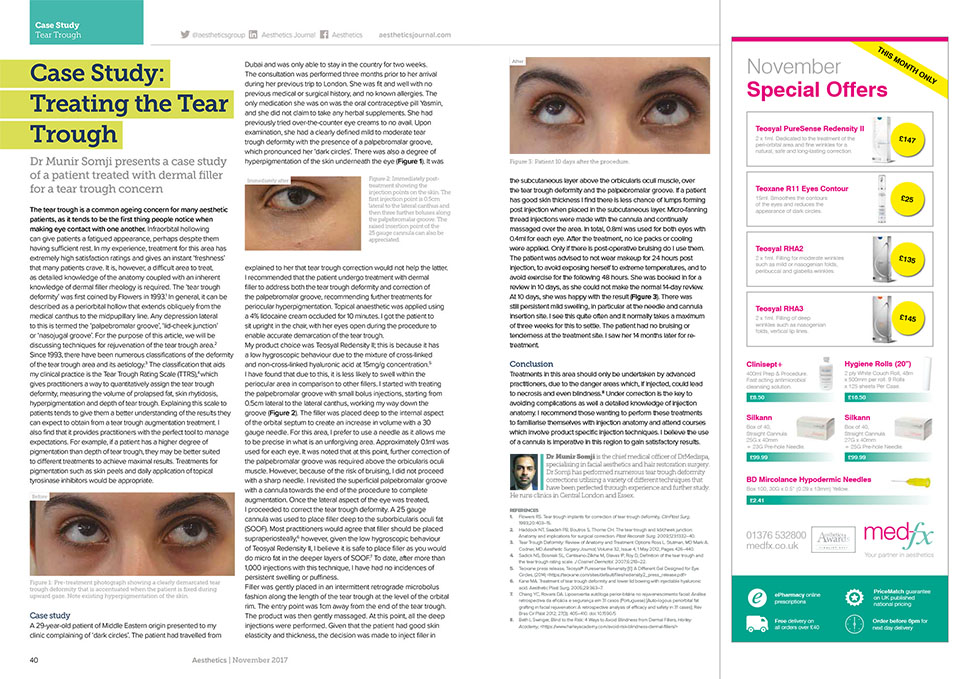
A 29-year-old patient of Middle Eastern origin presented to my clinic complaining of ‘dark circles’. The patient had travelled from Dubai and was only able to stay in the country for two weeks. The consultation was performed three months prior to her arrival during her previous trip to London. She was fit and well with no previous medical or surgical history, and no known allergies. The only medication she was on was the oral contraceptive pill Yasmin, and she did not claim to take any herbal supplements. She had previously tried over-the-counter eye creams to no avail. Upon examination, she had a clearly defined mild to moderate tear trough deformity with the presence of a palpebromalar groove, which pronounced her ‘dark circles’. There was also a degree of hyperpigmentation of the skin underneath the eye (Figure 1). It was explained to her that tear trough correction would not help the latter.
I recommended that the patient undergo treatment with dermal filler to address both the tear trough deformity and correction of the palpebromalar groove, recommending further treatments for periocular hyperpigmentation. Topical anaesthetic was applied using a 4% lidocaine cream occluded for 10 minutes. I got the patient to sit upright in the chair, with her eyes open during the procedure to enable accurate demarcation of the tear trough.
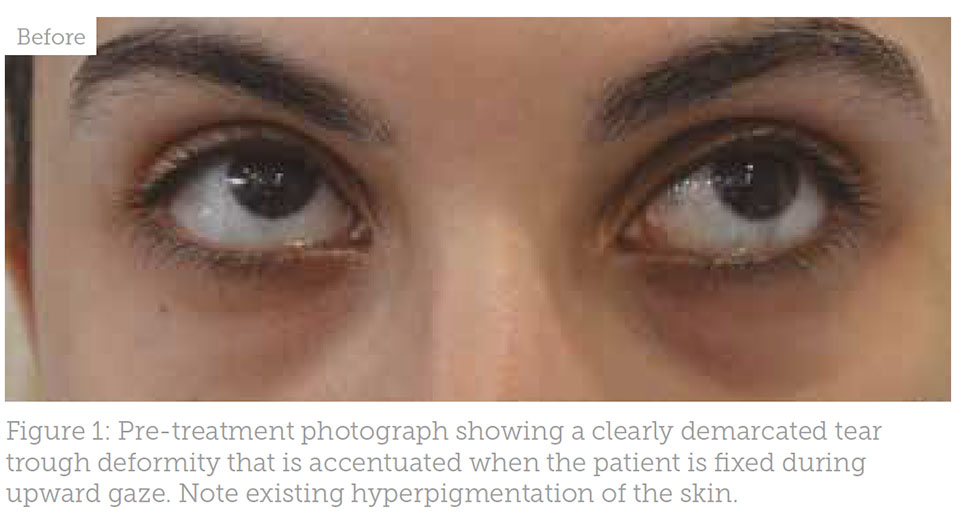
My product choice was Teosyal Redensity II; this is because it has a low hygroscopic behaviour due to the mixture of cross-linked and non-cross-linked hyaluronic acid at 15mg/g concentration.5 I have found that due to this, it is less likely to swell within the periocular area in comparison to other fillers. I started with treating the palpebromalar groove with small bolus injections, starting from 0.5cm lateral to the lateral canthus, working my way down the groove (Figure 2). The filler was placed deep to the internal aspect of the orbital septum to create an increase in volume with a 30 gauge needle. For this area, I prefer to use a needle as it allows me to be precise in what is an unforgiving area. Approximately 0.1ml was used for each eye. It was noted that at this point, further correction of the palpebromalar groove was required above the orbicularis oculi muscle. However, because of the risk of bruising, I did not proceed with a sharp needle. I revisited the superficial palpebromalar groove with a cannula towards the end of the procedure to complete augmentation. Once the lateral aspect of the eye was treated, I proceeded to correct the tear trough deformity. A 25 gauge cannula was used to place filler deep to the suborbicularis oculi fat (SOOF).
Most practitioners would agree that filler should be placed supraperiosteally,6 however, given the low hygroscopic behaviour of Teosyal Redensity II, I believe it is safe to place filler as you would do micro fat in the deeper layers of SOOF.7 To date, after more than 1,000 injections with this technique, I have had no incidences of persistent swelling or puffiness. Filler was gently placed in an intermittent retrograde microbolus fashion along the length of the tear trough at the level of the orbital rim. The entry point was 1cm away from the end of the tear trough. The product was then gently massaged. At this point, all the deep injections were performed. Given that the patient had good skin elasticity and thickness, the decision was made to inject filler in the subcutaneous layer above the orbicularis oculi muscle, over the tear trough deformity and the palpebromalar groove. If a patient has good skin thickness I find there is less chance of lumps forming post injection when placed in the subcutaneous layer. Micro-fanning thread injections were made with the cannula and continually massaged over the area. In total, 0.8ml was used for both eyes with 0.4ml for each eye. After the treatment, no ice packs or cooling were applied. Only if there is post-operative bruising do I use them.
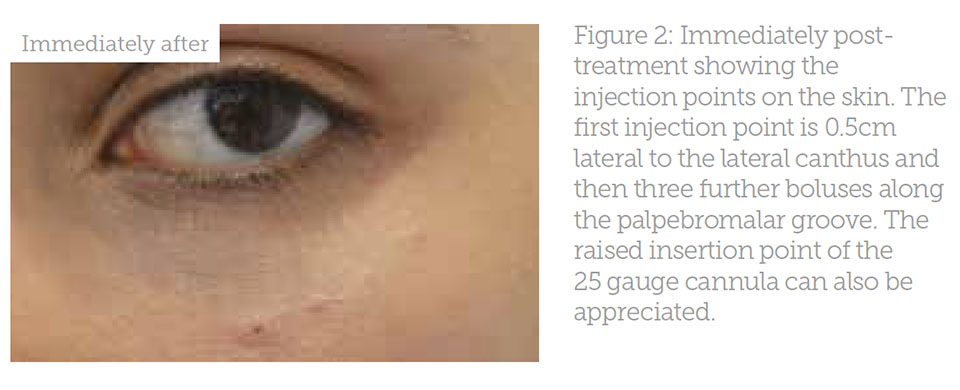
The patient was advised to not wear makeup for 24 hours post injection, to avoid exposing herself to extreme temperatures, and to avoid exercise for the following 48 hours. She was booked in for a review in 10 days, as she could not make the normal 14-day review. At 10 days, she was happy with the result (Figure 3). There was still persistent mild swelling, in particular at the needle and cannula insertion site. I see this quite often and it normally takes a maximum of three weeks for this to settle. The patient had no bruising or tenderness at the treatment site. I saw her 14 months later for retreatment.
Conclusion
Treatments in this area should only be undertaken by advanced practitioners, due to the danger areas which, if injected, could lead to necrosis and even blindness.8 Under correction is the key to avoiding complications as well a detailed knowledge of injection anatomy. I recommend those wanting to perform these treatments to familiarise themselves with injection anatomy and attend courses which involve product specific injection techniques. I believe the use of a cannula is imperative in this region to gain satisfactory results.
 Dr Munir Somji is the chief medical officer of DrMedispa, specialising in facial aesthetics and hair restoration surgery. Dr Somji has performed numerous tear trough deformity corrections utilising a variety of different techniques that have been perfected through experience and further study. He runs clinics in Central London and Essex.
Dr Munir Somji is the chief medical officer of DrMedispa, specialising in facial aesthetics and hair restoration surgery. Dr Somji has performed numerous tear trough deformity corrections utilising a variety of different techniques that have been perfected through experience and further study. He runs clinics in Central London and Essex.
REFERENCES
1. Flowers RS. Tear trough implants for correction of tear trough deformity, ClinPlast Surg. 1993;20:403–15.
2. Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: Anatomy and implications for surgical correction. Plast Reconstr Surg. 2009;123:1332–40.
3. Tear Trough Deformity: Review of Anatomy and Treatment Options Ross L. Stutman, MD Mark A. Codner, MD Aesthetic Surgery Journal, Volume 32, Issue 4, 1 May 2012, Pages 426–440.
4. Sadick NS, Bosniak SL, Cantisano-Zilkha M, Glavas IP, Roy D, Definition of the tear trough and the tear trough rating scale. J Cosmet Dermatol. 2007;6:218–22.
5. Teoxane press release, Teosyal® Puresense Renensity [II]: A Different Gel Designed for Eye Circles, (2014) <https://teoxane.com/sites/default/files/redensity2_press_release.pdf>
6. Kane MA. Treatment of tear trough deformity and lower lid bowing with injectable hyaluronic acid.
Aesthetic Plast Surg. 2005;29:363–7.
7. Chang YC, Rovaris DA. Lipoenxertia autóloga perior-bitária no rejuvenescimento facial: Análise retrospectiva da eficácia e segurança em 31 casos (Portuguese) [Auto-logous periorbital fat grafting in facial rejuvenation: A retrospective analysis of efficacy and safety in 31 cases]. Rev Bras Cir Plást 2012; 27(3): 405–410. doi: 10.1590/S
8. Beth L Swinger, Blind to the Risk: 4 Ways to Avoid Blindness from Dermal Fillers, Harley Academy, <https://www.harleyacademy.com/avoid-risk-blindness-dermal-fillers/>

